Fixing Fax Congestion in Pediatric Care: Early Lessons from Deploying a Faxless Intake Hub
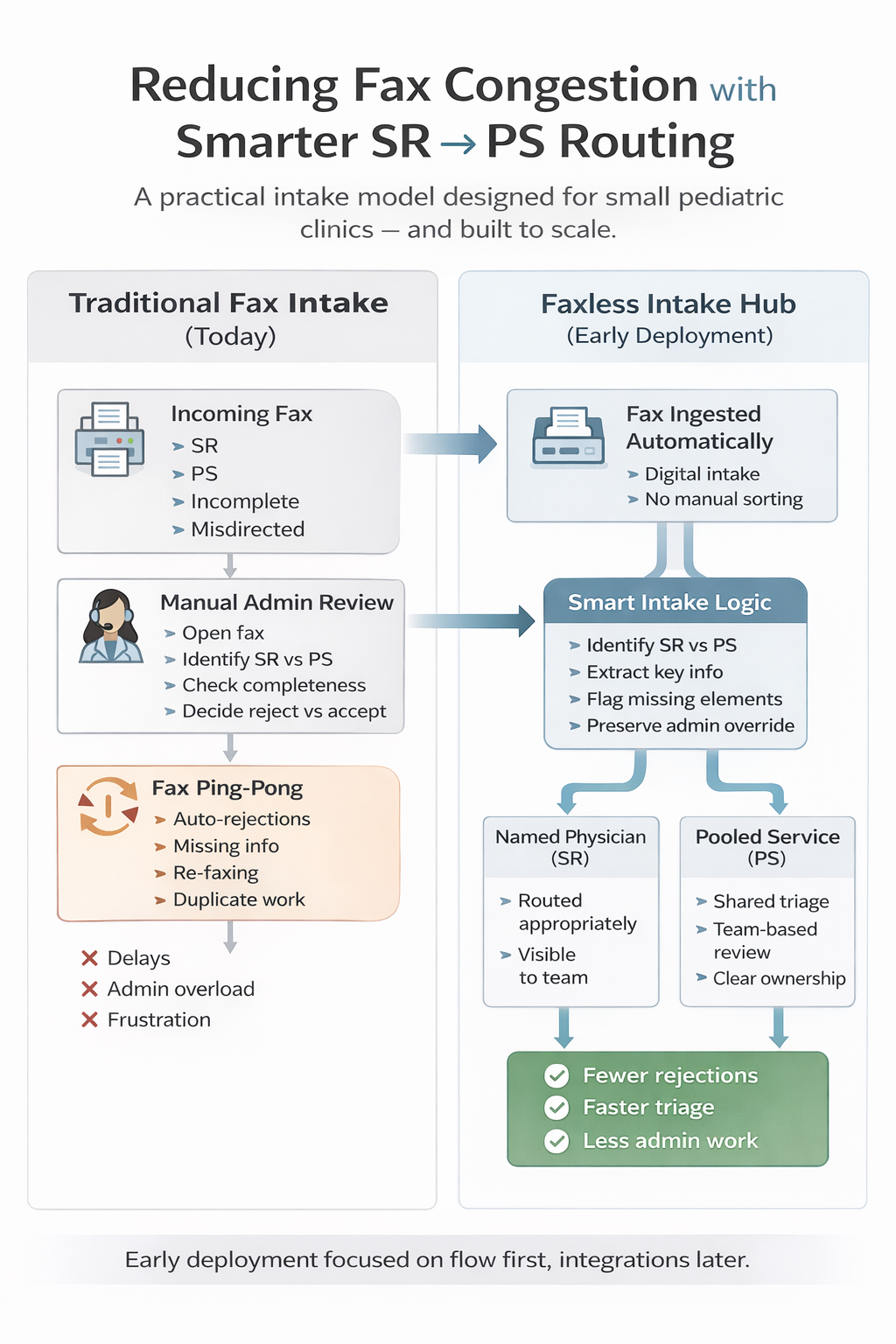
Despite years of discussion about digital health, fax remains the dominant intake method for referrals, consults, and supporting documentation in many pediatric clinics. For small offices in particular, this creates a daily operational burden that quietly drains staff time, delays care, and frustrates referring providers.
At Smart Clinic Systems, we've been working through this challenge by deploying a lightweight, faxless intake hub in a small pediatric setting — while intentionally designing it to support pooled services (PS), team-based triage, and future community collaboration.
This article shares what we're seeing so far, what's working, and why starting small — before deep EMR integrations — has been critical to adoption.
The Hidden Cost of Fax Congestion in Pediatric Clinics
In theory, fax is simple. In practice, it creates process congestion.
In a typical pediatric office, incoming faxes include:
- Specialist referrals (SR)
- Requests meant for pooled services (PS)
- Incomplete consults missing required forms
- Misdirected or outdated referral templates
- Duplicate or follow-up faxes triggered by rejections
Each fax requires manual review, categorization, and often a decision about whether it can proceed — or must be rejected and sent back.
This creates what many teams describe as "fax ping-pong":
- Referral arrives incomplete
- Admin identifies missing elements
- Fax is rejected with instructions
- Referrer resends (often incorrectly)
- Admin re-reviews the same consult again
The result:
- Increased admin workload
- Slower patient access to care
- Frustration for both sending and receiving clinics
- Higher risk of lost or delayed referrals
Why SR → PS Routing Is a Breaking Point
One of the most common failure points we observed is manual SR vs PS routing.
Admin staff are often responsible for determining:
- Is this referral to a named physician?
- Or should it be directed into a pooled / program service?
- Is it appropriate for the service at all?
When this logic lives only in human judgment — and varies by day, staff member, or workload — errors and delays compound quickly.
This is not a staffing problem.
It's a workflow design problem.
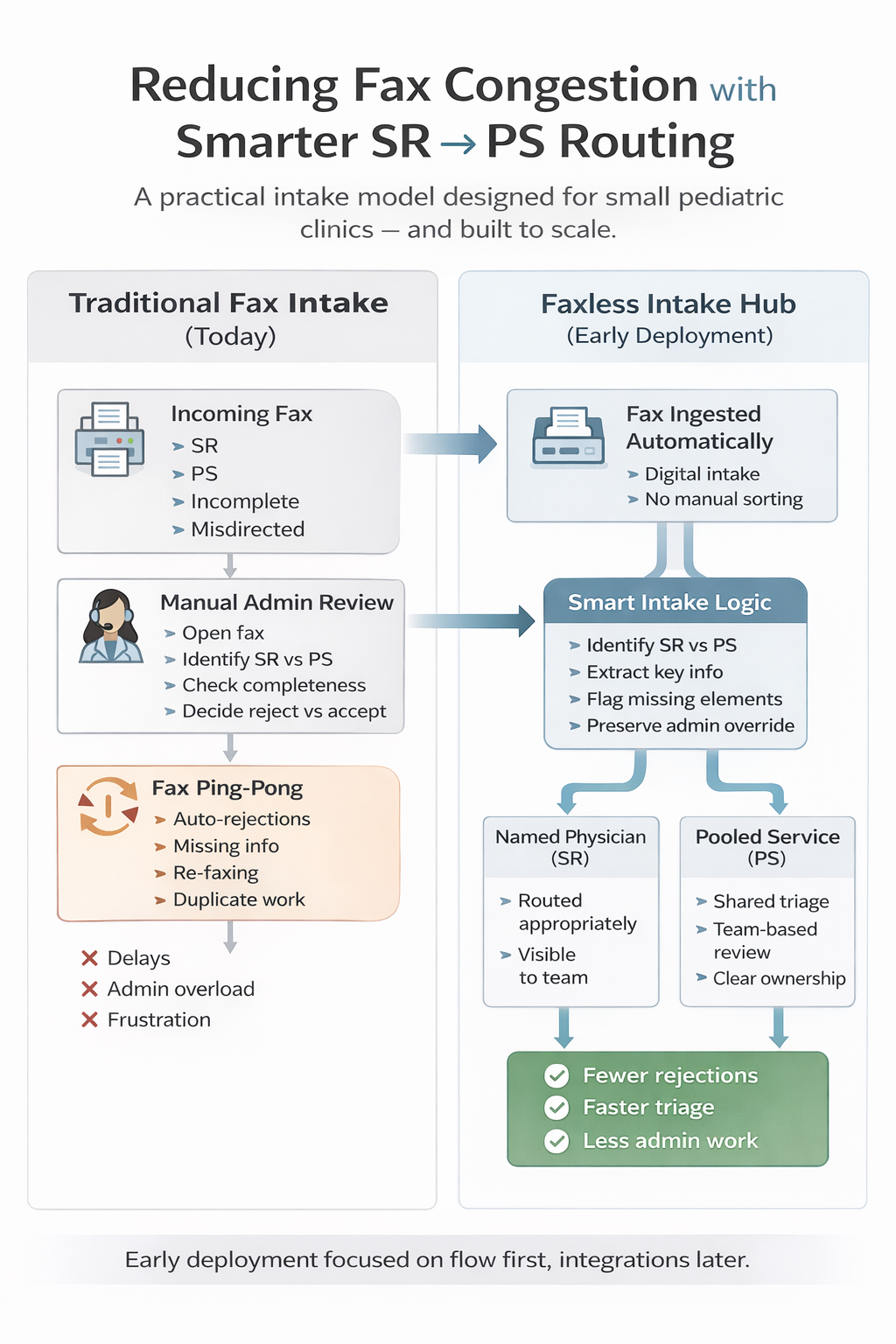
Our Early Approach: Reduce Friction First, Integrate Later
Rather than starting with deep EMR or PSS integrations, we took a different path:
Step 1: Remove unnecessary human sorting
- Automatically ingest incoming faxes
- Extract key referral metadata
- Identify referral type (SR vs PS)
- Flag missing or incomplete elements early
Step 2: Make the system useful on Day One
- No new logins required for most users
- Familiar workflows preserved
- Admin retains override and control
- Clear visibility into intake status
Step 3: Support teams, not just individuals
- Designed for a small pediatric office
- Works equally well for a single physician
- Built to evolve into pooled intake and collaborative hubs
- Allows shared triage without shared inbox chaos
This nimble deployment allowed us to earn trust quickly, reduce admin rework, and demonstrate value without asking clinics to overhaul their systems.
Early Signals of Traction and Adoption
Even in early stages, we've seen meaningful improvements:
- Fewer auto-rejections due to missing information
- Reduced back-and-forth with referring offices
- Faster identification of inappropriate referrals
- Clearer pathways for pooled vs named consults
- Less cognitive load on admin teams
Perhaps most importantly, staff feedback has focused less on "new software" and more on "this removed a step."
That's the signal we care about.
Designing for a Community, Not Just a Clinic
While our initial deployments focus on small pediatric settings, the architecture is intentionally designed for community participation:
- Pooled services across practices
- Shared intake logic without shared EMRs
- Gradual onboarding of additional clinicians
- Scalable governance without centralized bottlenecks
The goal isn't just to eliminate fax — it's to restore clarity and collaboration to referral workflows that have become fragmented over time.
What Comes Next
As adoption stabilizes, deeper integrations will follow. But our early experience reinforces a key lesson:
You don't fix fax problems by starting with integration.
You fix them by fixing flow.
Once flow improves, integration becomes a multiplier — not a prerequisite.
Final Thought
Fax congestion isn't a technology failure.
It's a signal that workflow design hasn't kept pace with clinical reality.
By starting small, respecting existing processes, and focusing on reducing unnecessary admin work, clinics can make real progress — today — while building toward a more collaborative, faxless future.